Treating the most serious cases of COVID-19 calls for the use of ventilators. We’ve all heard this, and also that there is a shortage of these devices. But there is not one single type of ventilator, and that type of machine is not the only option when it comes to assisted breathing being used in treatment. Information is power and having better grasp on this topic will help us all better understand the situation.
We recently wrote about a Facebook group focused on open source ventilators and other technology that could assist in the COVID-19 pandemic. There was an outpouring of support, and while the community is great when it comes to building things, it’s clear we all need more information about the problems doctors are currently dealing with, and how existing equipment was designed to address them.
It’s a long and complicated topic, though, so go get what’s left of your quarantine snacks and let’s dig in.
As we dig in, let’s address one common point of confusion in terminology: respirators are masks designed to protect the wearer, like keeping health workers from inhaling particles carrying Coronavirus, while ventilators are devices used by patients to help them breathe adequately.
How Our Lungs Work
 Image Source: Wikimedia Commons
Image Source: Wikimedia Commons
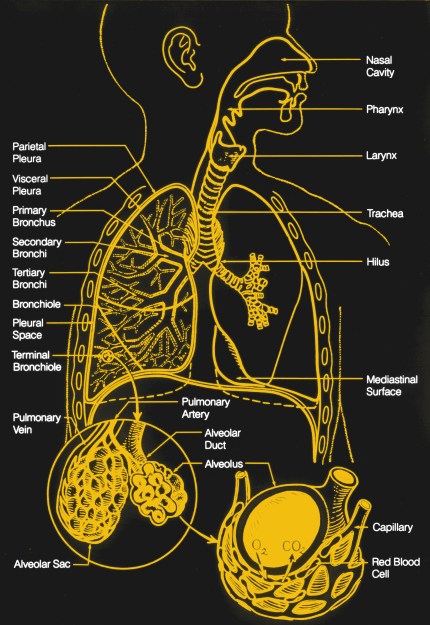
Our respiratory system does two things; it brings oxygen into the body, and it expels carbon dioxide from the body. It does this by taking air from atmosphere and passing it through smaller and smaller structures in the lungs, terminating in capillaries; these are tiny ‘veins’ that are able to pass individual molecules into and out of the blood stream.
The simplest way to imagine this respiratory system is as an inverted tree: a large trunk (the trachea) branches over and over again (bronchioles), ending in tiny leaves (alveoli) that perform the gas transfer. The alveoli are tiny structures like clusters of grapes and are covered in capillaries. The capillaries diffuse molecules of O2 into the bloodstream where they are carried around by blood cells, and take CO2 out. This mechanism is driven by pressure differences between the concentrations of O2 and CO2 in the blood cells compared to the air. The important part is surface area, as the more capillary surface area available to effect gas transfer, the better, which is why the lungs are a lot of tiny spheres instead of two giant cavities.
The gas transfer is assisted by respiration (breathing in and out). The body needs to constantly expel the carbon dioxide-rich air and bring in fresh oxygen-rich air, and this is done by changing the volume of the lungs. The diaphragm (underneath the lungs) and intercostal muscles (between the ribs) both perform work to expand the lungs. This increases the volume of the lungs and air rushes in to fill that volume in each of the small alveoli. Expiration is a mostly passive process; the muscles relax and return to their natural state, much like a stretched rubber band returning to its natural state. Active expiration requires effort from additional muscles.
There are little hairs called cilia and mucus-producing cells throughout the inside of this system. Their job is to capture waste and foreign particles that have been inhaled, and push them up and out, where they cross into the esophagus and the digestive system.
There are lots of things that can cause problems with this delicate system. If the branches are blocked, say with too much mucus, then there’s less surface area available for the gas transfer, and the person can’t get enough air with the same amount of breathing. If the bronchioles or capillaries become stiff (e.g. from smoking) or scarred, then it becomes difficult to squeeze the air out. If the lungs become damaged the alveoli can break down and the lung surface area is reduced, so diffusion is impaired. If the lungs become inflamed the airway is constricted and it becomes difficult to pass a large enough volume of air into and out of the lungs for gas transfer. If the person breathes too fast and moves a lot of air, or too slow and doesn’t move enough air, then their blood gas concentrations get out of whack. Too much carbon dioxide in the blood and the body becomes acidic, which is a problem that other organs then have to solve.
There are other problems that can happen in this system, such as the brain not getting the right signals about the amount of carbon dioxide and oxygen in the blood, or the brain being forgetful about telling the body to breathe. Those aren’t what’s happening with COVID-19.
Why Breathing Becomes a Problem
The CDC has a good guide on clinical management of patients that gives the stats on how the disease presents and what kinds of care they need. In patients that experience the worst symptoms of COVID-19, the problems are pneumonia (infection that leads to the lungs filling with fluid), dyspnea (difficult or labored breathing), and acute respiratory distress syndrome (ARDS). In simple terms, the patients can’t breathe well enough.
 https://commons.wikimedia.org/wiki/File:New_Pneumonia_cartoon.jpg
https://commons.wikimedia.org/wiki/File:New_Pneumonia_cartoon.jpg
The patient is struggling to breathe because the pneumonia is causing excess mucus production and cell infection, filling the alveoli and blocking the branches and reducing the surface area available for gas transfer. The alveoli that are accessible still work, but there aren’t enough of them available to sustain the patient. The result is labored breathing and insufficient gas transfer, which can lead to death.
According to the WHO, approximately 14% of the infected require hospitalization and oxygen support, and 5% require ICU admission. Looking at Bergamo, Italy, that 14% of the entire population is overwhelming hospitals, while in places that are better prepared, or where the curve is flattened, the health care system is stressed less.
The doctors in Italy are suggesting that the hospitals are becoming epicenters for virus transmission, and that home care may be preferred if possible, especially since they don’t have all of the resources they need. This is what’s causing the DIY community to look at ways to quickly develop some of those resources.
How We Provide Assisted Breathing
There are three main ways to help people who have difficulty getting O2 into their blood and CO2 out:
- Open up their airway to increase surface area
- Increase the oxygen content of the air
- Make it easier for them to breath in large volumes of air
Since air is 78% nitrogen, 1% argon, and 21% oxygen (with traces of other gases), there’s a lot of room for improvement in gas transfer by increasing the percentage of oxygen. Carbon dioxide diffuses a lot more easily than oxygen, so USUALLY it’s not a problem to get the CO2 out. At home this is done with an oxygen concentrator or delivered tanks. In a hospital this is done with central O2.
Another thing to do is to open up more of those passages and clear up the blockages and get at all those alveoli. One way to do that is the same way that works for sleep apnea; positive air pressure. By putting positive air pressure in all the branches, it helps keep those airways open just like gently blowing up a balloon keeps it from collapsing. The only thing is that the “balloon” we’re talking about here is made of delicate tissue that’s already stressed, and over-pressurizing is catastrophic.
We also help get more gas transfer to happen in the alveoli that are still accessible. This can be done by assisting the patient with the effort of inhaling, again with positive air pressure. In patients, labored breathing means they get exhausted just trying to get enough air, so assistance with the inhalation is necessary and this is often where ventilators become part of treatment.
The ultimate goal with these three things is to give the patient time to develop antibodies and fight the virus and clear out the lungs, so the patient could be on mechanical assistance for up to two weeks.
The Ventilator
The ventilator can help with these things. It doesn’t produce oxygen, but passes provided oxygen through it and to the patient. There are multiple kinds depending on the severity of the infection. Ideally you want NIV, or non-invasive ventilation which uses an external mask. Invasive ventilation requires a tracheostomy or endotracheal tube inserted in the nose or mouth down into the lungs, which is an incredibly difficult and risky process that can only be done by a qualified physician in a medical care setting and can lead to other complications.
 A CPAP machine creates heated, humidified, positive air pressure in the airway through a sealed face mask. By PruebasBMA – Own work, CC BY-SA 3.0, Link
A CPAP machine creates heated, humidified, positive air pressure in the airway through a sealed face mask. By PruebasBMA – Own work, CC BY-SA 3.0, Link
To best explain a ventilator, let’s start with a CPAP and work our way up. Short for Continuous Positive Airway Pressure, a CPAP takes normal air and compresses it and presents that higher pressure air through a hose to a mask. Usually the pressure is between 4-20cm H2O. If you’ve never used one, think about what it would be like to grow up in a swimming pool with your head above water, where your lungs are constantly pushing the water out of the way to breathe, and then after years you get out of the pool. Your muscles have to do a lot less work to bring in the air, and it rushes in easily. The CPAP is the same concept; by supplying higher pressure air, your lungs work less to inspire than they would otherwise and they can take deeper fuller breaths. More importantly, the pressure keeps the passageways from collapsing. Exhaling is a little more difficult, but remember that this is a mostly passive process; the natural elasticity of the lungs and muscles can overcome the increased pressure, within limits of course.
The BiPAP is the next level up. With some fancy sensing, it’s possible to detect the exhalation beginning, and then drop the pressure level down for the exhalation, making it easier to breathe out. You’ll see an IPAP and an EPAP number, which is the inhalation pressure, and exhalation pressure. Note that in both cases it’s still positive air pressure; we can’t have the passages collapsing on exhalation either. The other advantage is that with a greater difference in pressures, you can have a greater tidal volume (the amount of air that goes in and out in each breath, typically about 500mL or 7mL/kg of body mass) because the greater IPAP allows for more in, and the lower EPAP allows for easier expiration.
The ventilator is the next logical step. It can adjust the pressure either reactively or proactively, or both with special limits. For example, it could allow the patient to breathe on their own with BiPAP-like support, but ensures that the patient is breathing at least a certain number of breaths per minute, or it could take over the breathing process entirely and increase and decrease pressure at specific times to make the patient breathe when they couldn’t otherwise on their own.
Some ventilators are designed for home use, where the system vents the expired air directly from the patient, and the patient is relatively stable. With these ventilators the tube can be connected to a mask or to a tracheostomy tube.

Other ventilators are designed for acute hospital use. These have much more complex interfaces for the variety of treatment modes for which they are capable. They typically do invasive ventilation in which an endotracheal tube is inserted in the nose or mouth and down into the lungs. The biggest factor here is that the expired air is captured by the system and filtered before being released. In an application where the patient has a transmissible disease, this point is particularly important.
Most of these machines have an additional port that takes in supplied oxygen. This can be tanks, but not likely because of the high rate of flow needed. An oxygen concentrator can only supply about 10L/min. In the case of acute hospital ventilators, much more may be required. Most hospitals have central O2, capable of supplying up to 50L/min.
The Many Challenges of Ventilator Design
Now that you have the basics behind the tech, here are some specific challenges.
- You must have a good seal on the mask the person is wearing on their face. If you don’t have a good seal, the mask will leak and you won’t be able to maintain positive pressure. Poor sealing is one of the main reasons for these kinds of devices to fail.
- Monitoring expiration is important. The face mask must allow expired gases to leave, or else the patient will be rebreathing their own air. The machine knows how much it vents and takes that into account when supplying pressure. When the patient breathes out, the expired air doesn’t go into the machine, it goes out through the face mask vents and into the air. In a hospital environment, this would be aerosolizing the virus, which would be very bad, which is why the there are ventilator designs for hospitals that capture the expired air through a different tube and filter it.
- You have to maintain the level of positive pressure consistently; if there’s a leak you have to ramp up to maintain the pressure level, and if the leak is plugged you have to drop down immediately. If you go above the pressure level intended, you can easily do damage to the lungs. Pressures are typically in the 4-40cm H2O range. This is a big important requirement, because messing this one up does a lot of damage fast.
- You have to heat and humidify the air. Usually the sinuses do a good job of this, but on a ventilator, this isn’t possible because the sinuses may be bypassed. When the air is too dry, it can lead to hypothermia, bronchospasm, extra mucus production (which is bad because it blocks more passages), or other problems.
- With warm wet environments comes bacteria growth, and Legionnaires’ disease, a severe form of pneumonia caused by bacteria, is a serious risk in already compromised patients. Having an unsanitary environment could quickly cause problems worse than the original disease.
- You have to be able to supply a lot of oxygen. A portable oxygen concentrator (POC) won’t work for a couple reasons; First, it doesn’t pull out enough oxygen for the patients that have needed supplemental O2 so far. Second, it only dispenses oxygen when it detects breath, but since there’s positive air pressure going in, the sensors on the POC won’t work. Depending on the needs of the patient, a larger oxygen concentrator might be sufficient, but any ventilator design needs to allow for an oxygen inlet.
- The good news is that you only have to be able to supply positive pressure; ventilators do not suck the air out of the lungs. They merely provide varying levels of positive pressure and let the elasticity of the ribs and diaphragm take care of the exhalation.
- Either you’ll need lots of sensors (PaCO2, TcCO2, SpO2, FiO2 in addition to flow and pressure) and the ability to have complex algorithms, or you’ll need an expert constantly monitoring the patient. If they roll over and pinch the tube, or move and break the seal, or get agitated, or their condition changes in any way, it may be necessary to change the settings of the machine. The software that runs on existing devices is complicated, with good reason. You may not think about your breath rate throughout the day, but your body is regularly adjusting the amount of air it needs, and the system has to account for that.
- An adult male lung has a volume of about 5L, but tidal volume is roughly 500mL. This means that the system needs to be able to supply pressured air for at least 500mL per inhalation, and may need to keep applying pressure for the exhalation.
- Any design needs to be manufacturable using existing parts that are readily available. The reason for the shortage of ventilators now is that demand jumped faster than the manufacturers’ abilities to create product. They already have supply chains, manufacturing lines, injection molds, and working designs that are tested and proven. The only thing holding them back is their ability to source and assemble the components fast enough, and then distribute them, and you better believe they’re throwing every resource they can, with the assistance of every government, at solving all of the supply chain problems they have now. The entire point of flattening the curve is to give everyone as much time as possible to solve problems.
Using Ventilators Requires Highly-Skilled Health Care Workers
Besides the physical constraints of a machine, you need trained physicians to monitor the patients. IF you could get a DIY solution, these are the other things to consider.
- Each patient will need to be titrated and adjusted regularly. This is the process of figuring out what the right levels are for giving the patient treatment. There are multiple variables, like the inhalation pressure and exhalation pressure, whether the machine is leading the breathing cycle or the human, the rate, the sensitivity of the sensors. There is a huge risk of damaging the patient’s lungs through negligence. If the settings aren’t exactly right, then the patient could end up having to do more work fighting the machine than they would be doing without the machine, or have an improper blood gas balance. For example, if the EPAP setting is too high, the patient may be taking in more than they are exhaling, which is clearly not a sustainable solution.
- The same goes for O2 levels in the supplied gas. Since increasing the O2 levels can lead to flammable or explosive situations, it’s important that the system not leak and that there are sensors and protections in place to ensure that the O2 is going to the right place in the right amounts. Also, supplying too much oxygen can suppress the brain’s “drive to breathe” mechanism, the signal telling the respiratory system to breathe in and out, leading them to stop breathing.
- Cleanliness is essential, as it could cause issues worse than the original disease, and the ability to keep the machine clean even if it’s only used for a week, is critical.
- In most cases where a ventilator is needed, the patient has comorbidities (additional medical conditions) such as hypertension, diabetes, cardiovascular disease, and respiratory system disease (also here), which makes treatment more challenging.
- The biggest thing is that if the person’s conditions are so severe that they’re on a ventilator, then they’re going to need to be near immediate care, which means the solution has to be in a hospital setting. Even if we had a surplus of ventilators, the number of ICU beds and critical care staff would end up being the limiting factor.
- Any new device will require training of the caregiver, so it needs to work like existing units with which they are familiar, or be really easy to learn.
- It needs to be said that proper resource allocation is important here. We can’t have anyone hoarding ventilators for anticipated need while people are dying without them. Every ventilator that comes off a production line needs to go to a patient in need, and we should move them around as we can.
Current Manufacturing Efforts
The companies that make the necessary machinery are well aware of the problem and are ramping up production as quickly as they can. In addition to increasing production of the right kinds of ventilators, they are looking at CPAP and BiPAPs and non-life-support ventilators and exploring ways to take these medical devices with all of the appropriate safety mechanisms and certifications already in place and production lines already set up, and trying to find ways to adapt them to the specific needs for COVID-19.
One of their biggest problems right now is supply chain. China was shut down for a long time. Transportation routes are in disarray with airlines having fewer flights, countries closing borders, and even in the best of times shipping by sea takes a month. I know that GE has opened job postings for laborers to work on their assembly line in Madison, WI where I am writing this article, and I assume others all over the world are ramping up production to the best of their ability. Shifts are getting added, processes paralellized where possible, and injection molds warmed up. Setting up additional manufacturing lines might help, but it takes time to make all of the specialized equipment necessary. Even if new factories could retool quickly, the routing of components may be the more limiting factor and it’s quite possible that a specialized component will be a limiting factor for the entire industry. If production depends on a specific part, and an assembly line is already consuming that part as fast as it can be made, adding a second assembly line doesn’t “make the baby” any faster.
Some are looking into creative ways of multiplexing existing ventilators, just last week we saw Dr. Charlene Babcock demonstrate one way to convert a single ventilator for use with four patients based on a n emergency medicine feasibility study. As an exercise, try syncing your breath with someone near you and maintaining it. Even if you can get it to work for an extended period of time, you’d have to take into consideration that in a hospital all patients would have to be on all the same settings, with synchronized breaths of the same volume, they would all have to have the same resistance, and any change to any of them might mean that patient was no longer compatible with the other patients on the ventilator. Basically, it only works if you make them unconscious, and even then only briefly.
Conclusions
The DIY community is fantastic, and has a lot of bright people who are very capable of a variety of things. We’ve already seen 3D printed parts come to the rescue. Personal Protective Equipment (PPE) is being hacked together in rapid order by hackerspaces and 3D printing companies. Ventilators, though, are a whole new beast with a complexity similar to life support in a spaceship, though different enough that asking a car company to make one is like asking a ventilator company to retool to make a car. Asking a car company to make PARTS to help with supply chain problems makes sense, though. See the requirements put out by the UK for a ventilator solution for a more thorough guide to what’s needed.
My hope isn’t to discourage entirely; my hope is that this 101 will help guide a little so that effort isn’t wasted on solutions that can’t work. There’s an argument that “if there aren’t enough ventilators and patients are being turned away, I’d rather have a slim chance with a hacked solution than no chance with no solution. The reality is closer to “if there aren’t enough ventilators, a hacked solution will most likely do more damage than good, take up too much time from already strained health care resources, and could lead to death.” As the Hackaday community isn’t one for shying from a challenge, though, if you’re going to start somewhere, you should start with existing solutions that are close and in no short supply, like oxygen generators and BiPAPs and some kinds of ventilators, and look into how they could be modified without bypassing the safety mechanisms built into them, rather than start from scratch. As a community, we can and should help whenever possible. Let’s do it alongside the guidance of trained health professionals who have the skills to navigate the needs and the risks of assisted breathing.
This article was first featured at https://ift.tt/39oJDoB on March 25, 2020 at 10:06AM by Bob Baddeley





More Stories
Can this possibly be true? “Metal 3D printing is now possible on any 3D printer…with the right settings and a few minor upgrades like a hardened steel nozzle…” – July 2 2023 at 04:59PM
New NASA Funding Ignites 25 3D Printing Projects in Space Exploration – June 18 2023 at 04:34PM
Nvidia AI produces 3D models from 2D videos 3D printing applications forthcoming? – June 15 2023 at 02:55AM